Endometrial polyps, benign nodular protrusions of the endometrial surface, demand our attention as they contribute to endometrial thickening differentials. Sessile or pedunculated, these growths can be suggested on initial ultrasound or MRI studies, but confirmation may require more detailed approaches.
Epidemiology and Risk Factors:
With prevalence increasing with age (8-35%), endometrial polyps are not uncommon. Various risk factors, from tamoxifen use to chronic cervicitis, amplify the likelihood of their occurrence.
Clinical Presentation and Pathology:
Mostly asymptomatic, these polyps can manifest as a common cause of postmenopausal bleeding. In premenopausal women, they may lead to intermenstrual bleeding, metrorrhagia, and infertility. Histologically, polyps exhibit local hyperplastic overgrowths of glands and stroma, with a small percentage showing premalignant or malignant potential.
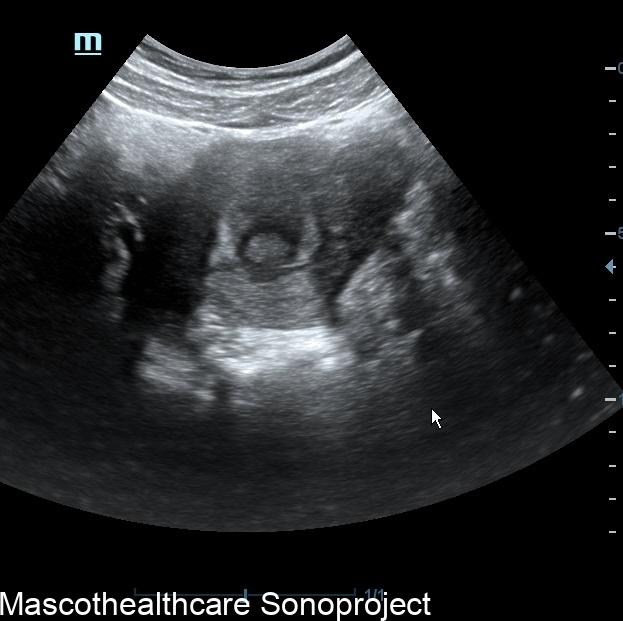
Location and Radiographic Features:
Predominantly found in the fundal and cornual regions of the uterus, these polyps can be multiple in about 20% of cases. Imaging through Hysterosalpingography (HSG) may reveal filling defects, but ultrasound remains the preferred method. Postmenstrual ultrasound unveils solitary, homogeneous, and echogenic lesions. The "interrupted mucosa sign" becomes a hallmark, indicating a disruption in the normal mucosal contour.
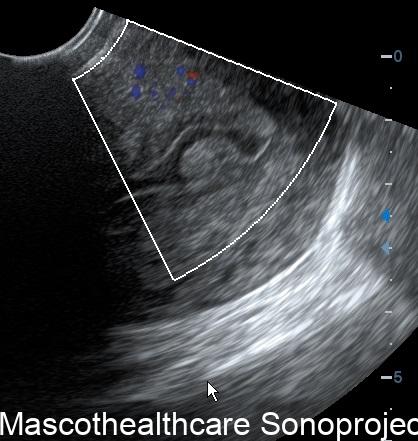
Nuances of Ultrasound Imaging:
The "bright edge sign" introduces short echogenic linear echoes at the polyp borders, contributing to a distinct appearance. Stalk characteristics, whether thin or broad-based, further aid in differentiation. Rarely, polyps can mimic endometrial hyperplasia or appear as diffuse endometrial thickening. Color Doppler imaging reveals a feeding artery sign, emphasizing the vascular nature of these growths.
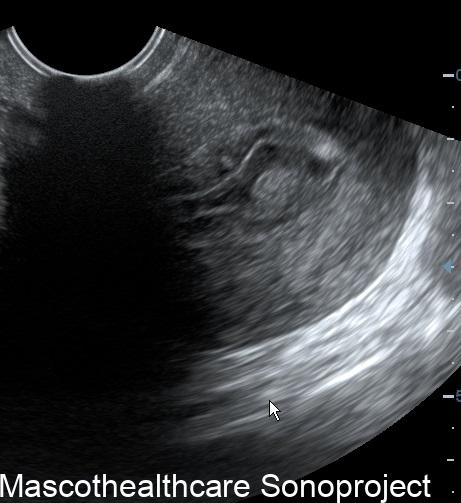
Sonohysterography: A Detailed View:
While not always necessary for diagnosis, sonohysterography emerges as a powerful tool. Polyps appear as echogenic, smooth, intracavitary masses outlined by fluid. This method provides a well-defined, homogeneous, polypoid lesion that is isoechoic to the endometrium, preserving the endometrial-myometrial interface. A well-defined vascular pedicle within the stalk solidifies the diagnosis.
Treatment and Prognosis:
Fortunately, most endometrial polyps are benign and can be treated with a polypectomy if symptomatic. Complications such as prolapse are rare, and the chance of malignancy is minimal.